Cardiologists reveal key ways to identify a heart attack and share vital steps to manage one with care.
A heart attack is a blockage of blood flow to the heart. When the heart doesn’t get enough oxygen, it can become life-threatening. Heart attacks are medical emergencies that shouldn’t be ignored and should be addressed as soon as possible.

The chances of surviving a heart attack or saving a life depend on several factors, but what matters most is being able to identify when one is taking place and remembering five steps. As the weather gets warmer, health issues that you may not be aware of may flare up. To be prepared, read on for life-saving tips for heart attacks.
Learn more about heart health tips by reading how to check your heart metrics at home, six important blood tests to take and understanding the importance of your blood type.

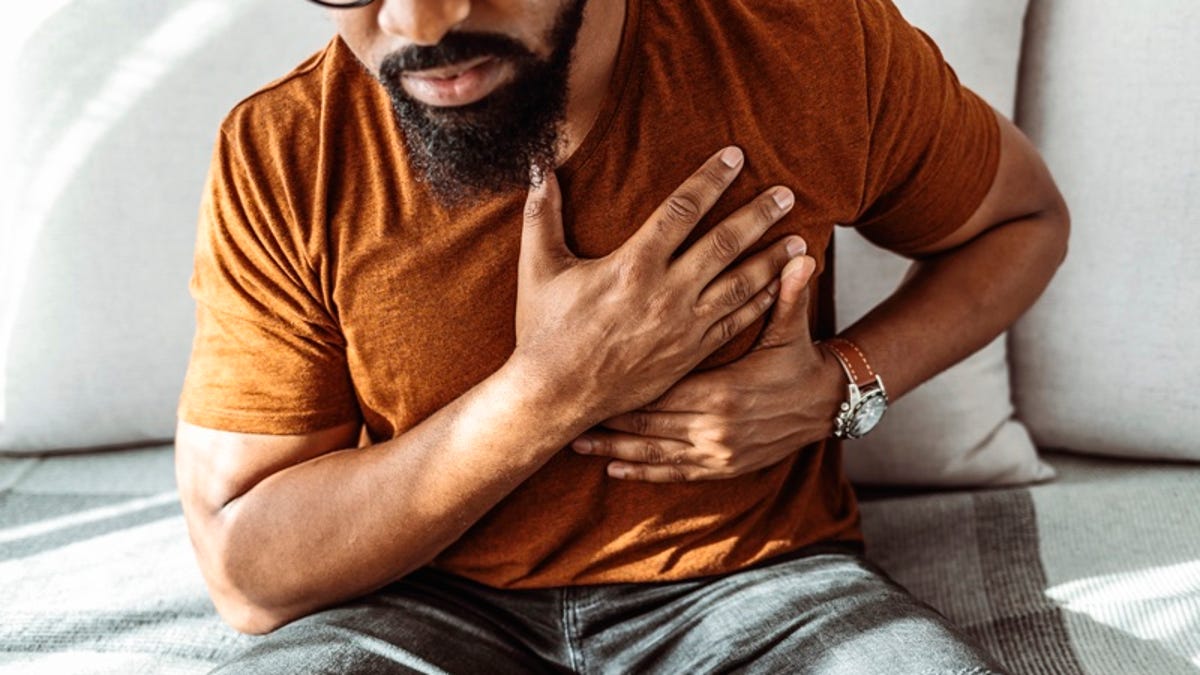
Common symptoms of a heart attack
When you think “heart attack,” classic symptoms such as chest discomfort might first come to mind. Heart attacks can present differently in men and women and in people with certain diseases, like diabetes.
Heart attack symptoms could include:
- Chest discomfort, pain or pressure that radiates up to your jaw, your back and/or your left shoulder
- Bad indigestion or nausea
- Extreme fatigue
- Shortness of breath
- Feeling generally unwell
“Essentially anything from the belly button up,” says Dr. Khadijah Breathett, a heart failure transplant cardiologist and tenured associate professor of medicine at Indiana University. “Constant pressure should raise concern that you should see your doctor, and it’s OK if it’s something else. We’d rather have an individual come see a health care professional and get evaluated rather than toughing it out at home, because that is what contributes to the escalating risk of death.”
1. Call 911, no matter what
If you feel any of the above symptoms, even if you aren’t sure it’s a heart attack, you should call 911 immediately, doctors recommend.
“If you feel unwell, or you’re starting to have chest discomfort, seek medical attention quickly, because the sooner you get treated, the better,” says Dr. Grant Reed, an interventional cardiologist and director of Cleveland Clinic’s STEMI program. “A lot of patients ignore their symptoms, and by the time they come in, their heart muscle has already died.”

The No. 1 indicator of how well you’re going to do after a heart attack is how fast you recognize your symptoms, Reed adds. There’s a strong relationship between when you start to have your heart attack (which is generally when symptoms start) and how fast doctors can open up the blocked coronary artery that’s causing it — the shorter the time, the better the outcomes, not just regarding survival but also the likelihood of heart failure or needing to be readmitted to the hospital.
When you get to the hospital, medical professionals will likely perform an electrocardiogram, which will determine the diagnosis of a heart attack. If it is a heart attack, you’ll be taken to the cardiac catheterization laboratory, where a coronary angiography will be performed. If you have a blockage in your coronary artery, the doctors will offer treatment with a balloon and a stent to keep the artery open.
Many people are hesitant to seek emergency medical care due to a lack of insurance or immigration status. In the US, hospitals are required to treat all people who come in with life-threatening emergencies.
“It’s a lot better to be treated and deal with the financial ramifications after the fact,” Reed says. In most cases, costs can be sorted out with the hospital, he adds.
2. Have an ambulance take you to the hospital
If you suspect you’re having a heart attack, don’t drive yourself to the hospital: Call an ambulance. You could lose consciousness and hurt yourself or others on the road, says Dr. Joel Beachey, a cardiologist at Mayo Clinic Health System in Eau Claire, Wisconsin. The same goes for having a loved one drive you — if your symptoms worsen, they won’t be able to help you while they’re driving, and may be distracted.
Paramedics can provide the best and fastest care while you’re on the way to the hospital, including giving you an assessment and providing some treatment, Beachey says.
If you’re with someone who is having heart attack symptoms and becomes unconscious, you should first call 911 and then engage in CPR, Breathett says. (You can find free CPR training at your local American Heart Association branch and many other places.)
3. Take aspirin, if you have it
If you’re having heart attack symptoms and have access to aspirin, take a full dose of 325 mg after calling the ambulance, Beachey says. (If you have baby aspirin, which comes in an 81 mg dose, take four of those.) He recommends chewing it instead of swallowing, so it gets into your system faster.
The reason? When you’re having a heart attack, a plaque inside your arteries becomes unstable and ruptures, which forms a blood clot that can close off supply to that artery. Taking aspirin can help break down some of that blood clot.
Aspirin for Heart Disease Prevention: What the New Guidance Means


4. Advocate for yourself
In an ideal world, healthcare providers would take all patient concerns seriously when it comes to heart attack symptoms, but studies show women and people of color are less likely to receive adequate treatment for heart attacks and heart disease. For example, older Black women were 50% less likely to be treated when they arrived at a hospital with a heart attack or coronary artery disease symptoms than white women, including after accounting for education, income, insurance status and other heart health complications like diabetes and high blood pressure, a 2019 study found.
“It’s been very clear over most of our history in the US that women and people of color are not heard,” Breathett says. “Their symptoms get dismissed, and they have worse outcomes. As a health care system, we have a lot more work to do to change that system so that each person can get equitable care irrespective of their demographic.”
Until that time comes, patients need to be their own advocates and speak up for themselves, she adds. If they aren’t being heard, they have the right to seek care elsewhere.
One tip recommended by a resident on TikTok: If you feel a provider isn’t taking your symptoms seriously, for heart health or otherwise, you can ask the provider, “What is your differential diagnosis?”
@dor_the_graytPOCs are more likely to be ignored. Ask questions, take notes, document the events. If you are alone, have a relative/friend on the phone.#patientadvocate#racisminmedicine#maternalmortality#bipoc#blackwomen#learnontiktokoriginal sound – Dorender Dankwa
A differential diagnosis is a term to describe what the different diseases are that could be contributing to your symptoms, basically asking the provider to explain why they’ve ruled out a heart attack and what else it could be. “That might help a person realize, oh, I haven’t effectively tested to make sure this is not cardiac disease,” Breathett says.
You can also bring a family member or friend to help ask questions on your behalf. Write down questions in advance if you can, so you can have them addressed during your short visit. And call back with any questions that weren’t answered. If you’re not satisfied or feel that you’re not being heard, seek out another care team.
5 Heart-Healthy Foods to Add to Your Grocery List This Week

5. Work on prevention
You’ve heard it a million times, but that’s because it’s true: The best way to prevent a heart attack is by maintaining a healthy diet, doing moderate exercise for 120 to 150 minutes per week, keeping your cholesterol and blood pressure under control and not smoking.

Heart attacks can happen to people of any age, race or gender. You should get regular physical exams with your primary care provider to assess your risk and make lifestyle changes that can help with prevention. Some people might also benefit from taking a baby aspirin every day as a preventative measure, but you’ll need to talk to your care provider about that.
Exercise is important even if you have a history of heart trouble, Beachey says.
Knowing what to do to prevent and respond to a heart attack is just one of the many important elements of your health you should know about. Read on to discover the best workouts to strengthen your heart, the difference between the types of cholesterol and how your diet affects your health. Plus, if you’re looking for new ways to monitor your metrics, check out CNET’s list of recommended fitness trackers and blood pressure monitors.
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.
Other Wellness Guides
Personal Care
Sleep
Fitness
Nutrition
Medical and Mental Health
Social Security Disability Insurance: How To Check Your Eligibility and Apply
Thinking of applying for Social Security Disability Insurance? Here’s how to check your eligibility and apply.

Blake Stimac
April 28, 2025 11:17 a.m. PT
4 min read

Social Security Disability Insurance, or SSDI, is a program that provides monthly payments to disabled workers, adult children and widows or widowers. The program requires a qualifying diagnosis that prevents an individual from working for at least a year or a diagnosis that is expected to result in death.
However, just meeting the minimum requirements doesn’t automatically guarantee that you’ll receive SSDI. Instead, applicants must provide a considerable amount of evidence to confirm qualification, and the process itself can take a long time. Below, we’ll fill you in on the details for eligibility and how to apply for SSDI.
For more, check out the Social Security payment schedule for the month and the Supplemental Security Income payment schedule.
What conditions qualify for Social Security Disability Insurance?
Qualifying for SSDI isn’t so cut and dried as you might think it could be. Given the variety of ailments that could keep you from working, there’s no set-in-stone list that will automatically disqualify you if you don’t check all or even some of the boxes. However, some specific conditions automatically qualify as long as you meet the proper diagnosis requirements.
The Social Security Blue Book, or Disability Evaluation Under Social Security, is a directory that details approved disabilities. For adults, they’re broken down into 14 categories.
- Cancer (Leukemia, lymphoma, multiple myeloma, breast cancer and prostate cancer)
- Cardiovascular system (congenital heart disease and heart failure)
- Congenital disorders that affect multiple body systems (non-mosaic Down syndrome)
- Digestive disorders (bowel or liver disease)
- Endocrine disorders (diabetes, thyroid disease, hyperglycemia and hypoglycemia)
- Genitourinary disorders (chronic kidney disease)
- Hematological disorders (sickle cell anemia, thrombosis and hemophilia)
- Immune system disorders (HIV, inflammatory arthritis and lupus)
- Mental disorders (bipolar disorder, dementia, depression and intellectual disabilities)
- Musculoskeletal disorders (spinal disorders or amputations)
- Neurological disorders (Parkinson’s disease, epilepsy, multiple sclerosis and traumatic brain injuries)
- Respiratory disorders (asthma, cystic fibrosis and chronic obstructive pulmonary disease, aka COPD)
- Skin disorders (burns, dermatitis and ichthyosis)
- Special senses and speech (impaired hearing, sight and speech)
For children, the same categories apply, and low birth weight (LBW) and failure to thrive (FTT) are included. Qualification for children is slightly different, as there’s no need for proof that the disability can prevent them from working. Instead, proof that the condition imposes a severe functional limitation for at least a year or is likely to be the cause of the individual.
How do I apply for Social Security Disability Insurance?
Before you apply for SSDI, make sure you have everything ready for the process. You’ll need ample documentation about your disability, diagnosis and employment history. Gather everything you can beforehand so you aren’t scrambling for it later.
You can apply for Social Security Disability Insurance online, over the phone at 1-800-772-1213, or by stopping by a local Social Security Office. If you opt for the office visit, it may be beneficial to call ahead of time, as you’re more than likely to need an appointment.
If you’ve applied for SSDI within the last 60 days and were denied, you will automatically be denied again, so exercise patience during the process. Applicants can also not already be receiving Social Security benefits prior to applying to SSDI.
Updated identity proofing measures
In late March, the Social Security Administration announced that it would be adding certain restrictions to it’s identity proofing policy in some cases if a person cannot apply online. It later walked back most of the restrictions and all claims can be completed over the phone after passing an anti-fraud check. However, the SSA will flag potentially fraudulent accounts, which will require an identity proofing checking in person.
Additionally, if you’re currently receiving benefits and need to update your direct deposit information and are unable to complete the task using a My Social Security account, it will have to be completed in person. If you find yourself in this situation, you can call the SSA to schedule an in-person appointment.
What could cause my SSDI application to be denied?
Between 2010 and 2019, the average denial rate of SSDI benefits was 67%. There are several reasons why your application could be denied, and below is a short list of factors that could contribute to a denial.
- Applying again after denial instead of submitting an appeal
- Insufficient medical evidence to support disability diagnosis
- An impairment that is not expected to last 12 months
- An impairment that is not considered severe
- Applicant is able to perform his or her usual type of work
- Applicant is able to perform another type of work
The applicant has an impairment resulting from:
- Drug addiction
- Alcoholism
Or, the applicant:
- Fails to cooperate
- Fails to follow prescribed treatment
- Does not want to continue development of the claim
- Returns to substantial work before disability can be established
Are there additional programs outside of SSDI?
Social Security Disability Income recipients may also qualify for Supplemental Security Income benefits if they meet certain criteria. In an agency report from 2022, the SSA revealed that about one in 10 SSDI recipients also had SSI as an additional source of income.
Funded by the Treasury Department and administered by the SSA, Supplemental Security Income also has strict requirements for qualification. It generally is provided to those who have low income and resources. And while SSDI is a benefit that’s earned through Social Security taxes deducted through the course of your employment history, SSI is not, and you can still qualify if you’ve never worked or paid Social Security taxes.
While the 2024 maximum payout for SSI recipients is $943 for an individual and $1,415 for a couple, other factors can reduce your monthly benefit. Your income, your living situation and certain family members’ income can affect your SSI payment.
Learn how to check your eligibility and apply for Supplemental Security Income.
For more on Social Security, find out if you have to pay back a Social Security overpayment and four ways you could lose your Social Security benefits.
 Why You Can Trust CNET
Why You Can Trust CNET
Our expert, award-winning staff selects the products we cover and rigorously researches and tests our top picks. If you buy through our links, we may get a commission. Reviews ethics statement
Is My Nonstick Cookware Safe or Does It Cause Teflon Flu? Here’s Everything We Know
“Forever chemicals” are more than just a buzz. If you’re not careful with your nonstick pots and pans, they can do more harm than good.

May 1, 2025 7:37 a.m. PT
6 min read

Teflon-coated or nonstick cookware sets, regardless of how you know them, are appreciated for how easy they are to use and clean. However, some circles also dislike these chemical-coated utensils. More specifically, the PTFE and PFAS (used in the coating) that are said to mix with your food during use earn them a bad rep.
Last year, the US saw an increase in reported cases of Teflon flu — if that raises questions in your mind, you’re not alone. Several Reddit users expressed the same concerns, with some wondering whether inhaling Teflon fumes while cooking is dangerous. The good news is that if your cookware was made after a particular year and you use it properly, you should be in the clear.
Read more: Never Raise Your Air Fryer Above This Temperature
Here’s what you need to know about Teflon flu and using your nonstick kitchenware without health worries.
What is Teflon flu?

The chemical polytetrafluoroethylene (PTFE), found in Teflon and similar nonstick surfaces, is common in air fryers, pots and pans and other kitchen appliances. When these materials overheat, they can release synthetic compounds that pose health risks.
Polymer fume fever, or Teflon flu, has reignited a debate about nonstick cookware safety. The illness occurs when fumes from an overheated Teflon or nonstick pan are inhaled. Nonstick pans are made with polytetrafluoroethylene (also known as PTFE). PTFE’s are known as “forever chemicals” since they take decades or sometimes even hundreds of years to break down.
Read more: I Upgraded to This PFAS-Free Glass Fryer and You Should, Too
Under normal use, PTFE’s aren’t thought to cause a health risk, but when heated to above 500 degrees Fahrenheit there are increased emissions and the resulting polymer fume fever. Polymer fume fever causes a range of reported symptoms including fever, chills, muscle tension and headache. Symptoms of Teflon flu are temporary and generally start within 12 hours of exposure, but can take up to 24 hours to take hold.
Best Nonstick Frying Pans, Tested and Reviewed

How to avoid Teflon flu
Teflon and nonstick cookware is easy to use, clean and maintain but it should only be used for low to medium heat cooking. Never heat your nonstick cookware over high heat or medium heat for long periods of time. Try to keep the surface temperature at or below 450 degrees Fahrenheit, or emissions from the PTFE coating are likely to increase.

What is Teflon and does it cause cancer?
Nonstick or Teflon is a popular choice for home cooks. The biggest advantage is that food won’t stick to pots and pans coated with Teflon the way it does to other metal materials, so it’s easy to flip a pancake or remove a cooked egg. Nonstick is also very easy to clean, generally taking no more than a few seconds to wash by hand.
Teflon is a brand name for a synthetic chemical called polytetrafluoroethylene that’s used in many household products, from wire coatings to fabric protectors and kitchen cookware, too. The knock on Teflon is that it’s unsafe if consumed or absorbed into the body and can increase the chances of cancer and other diseases. Studies have shown some connections (more on that below), but Teflon still exists and is used to make cookware, and the safety concerns around Teflon are mostly a thing of the past.
I stress mostly. Here’s why…
The brand Teflon may be associated with a risk of cancer, but it’s actually a chemical formerly used in the making of Teflon called PFOA that’s to blame. According to the Centers for Disease Control and Prevention, perfluorooctanoic acid is a manufactured perfluorochemical developed in the 1930s and used to make fluoropolymer coatings and products that resist heat, oil, stains, grease and water.

What are the negative effects of PFOA?
In some studies, PFOA has been linked to cancer, immune deficiency and a host of other medical problems. It has also been shown to affect growth and development and injure the liver in laboratory animals.

As recently as 2017, chemical giant Dupont settled a lawsuit for more than $670 million for its role in contaminating drinking water with PFOA (also referred to as C-8) in the mid-Ohio Valley. A previous class-action suit from 2004 in the same area led to a study that found PFOA was linked to cancer and compromised immune function, even in small doses.
Teflon cookware made before 2013 may be toxic
All that was enough for most manufacturers to halt the production of nonstick coatings using PFOA around 2002. Teflon using PFOA wasn’t officially banned in the United States until 2014. Europe banned it in 2008. That means if you own Teflon nonstick cookware from 2013 or earlier, there’s a chance it contains PFOA. Nine years is typically longer than the average lifespan of a nonstick pan, but if you’re not sure, it’s probably best to replace any Teflon-coated pots or pans.
If you’re concerned, look for PFOA-free cookware
Because of the ban, all nonstick cookware made in the US should be PFOA-free, but you’d be wise to make sure. Be extra cautious about buying cheap or off-brand cookware, especially if it’s not produced in a country with an active PFOA ban. PFOA is still produced elsewhere, largely in China, and used to make consumer products.
The good news is that PFOA-free nonstick cookware is cheap, so there’s no reason to risk it with anything that might contain the chemical. You can nab a 10-inch skillet from a trusted cookware brand like Misen for $99 or Tramontina for around $30. Luxury cookware brand All-Clad makes a two-piece nonstick cookware set for $60.

The best natural nonstick cookware alternatives
If you’re ready to ditch Teflon and chemical-based nonstick pots and pans altogether, there are plenty of more natural nonstick alternatives.
The most nonstick of the bunch is ceramic cookware, which has seen a boom in popularity since concerns about Teflon first surfaced. A few popular ceramic cookware options include The Always Pan (read my full review here), Caraway and Greenpan.
Cast iron is another cookware material that develops a natural nonstick coating over time, especially if you season it well and care for it properly. It won’t likely ever become as nonstick as Teflon, but cast iron has loads of other culinary benefits that are worthy of a few extra seconds of scrubbing in the sink after use. Lodge is a tried-and-true cast-iron cookware producer: You can scoop up a 10-inch skillet for as little as $20.

Carbon steel is yet another option and functions similarly to cast-iron cookware, although it’s not quite as heavy, slightly more sensitive to corrosion, and typically more expensive. Carbon steel hasn’t really popped off here in the US but is a favorite of professional chefs, as well as yours truly. Cookware startup Made In produces some excellent carbon steel cookware with prices starting around $89, but there are cheaper options out there.
FAQs
Should I worry about buying Teflon nonstick cookware?
The Teflon brand stopped using PFOA, the offending chemical behind Teflon flu, in 2013. That means that it should be safe to use new Teflon cookware any way you see fit — though it couldn’t hurt to continue being cautious when using new nonstick cookware.
Can I only catch Teflon flu from Teflon products?
No. The name Teflon flu originates from the Teflon brand because they famously used PFOA chemicals in the process of creating its cookware before 2013. However, that doesn’t mean your cookware is PFOA-free. If your cookware is created in the US, it should be free of harmful chemicals. But cheap companies and off-brands that create cookware in countries without PFOA bans often still use the chemical in their products, and those might still wind up in your hands.
How common is Teflon flu?
Teflon flu is not incredibly common, but there are still a significant number of cases reported each year. In 2023, there were 267 reported cases in the United States, the most since 2000, according to America’s Poison Control centers. The National Capital Poison Center also states that incidents of Teflon flu are likely underreported, as symptoms often appear hours after exposure and can mimic the common cold.
DATE . May/7/2025


